Strategic Consulting.
Strategic Consulting.
All we Need:
All we Need:
Your claims and the contracts that govern them.
From there, we evaluate how:
The benefit is designed
How it operates
Where value is gained or lost.
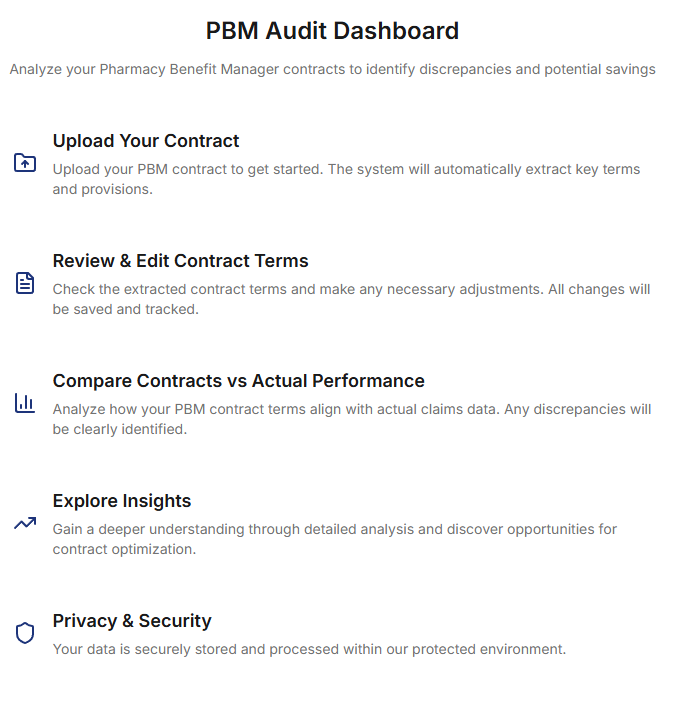
Audit Function
Reprice in Minutes
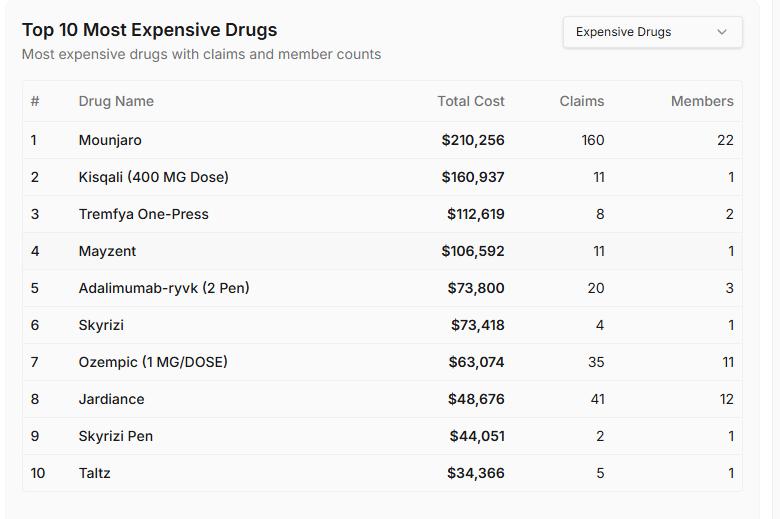
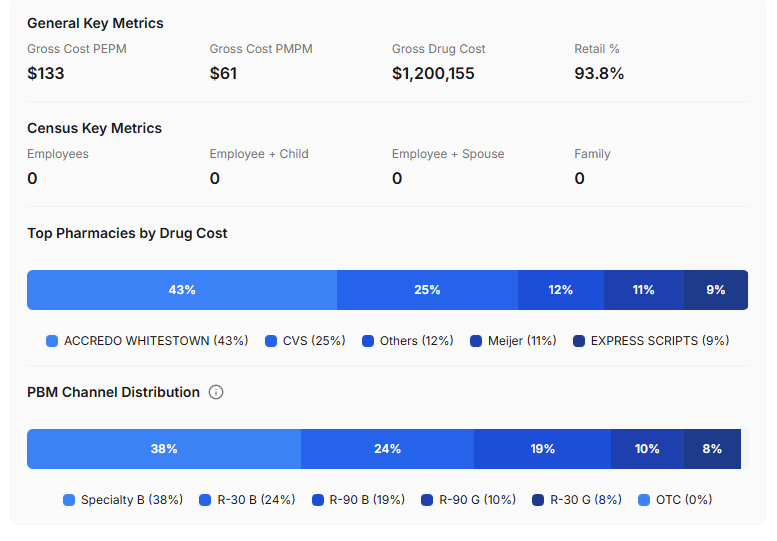
Top 10 Drug Spend
Utilization Analysis
Drug Channel Analysis
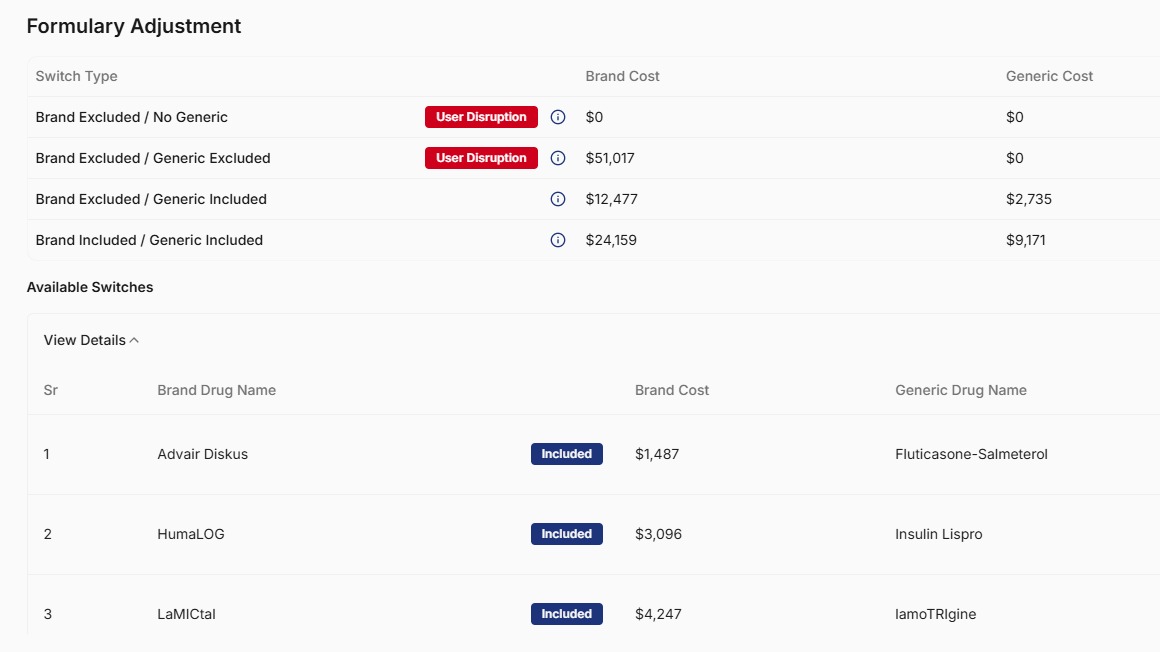
Disruption Report
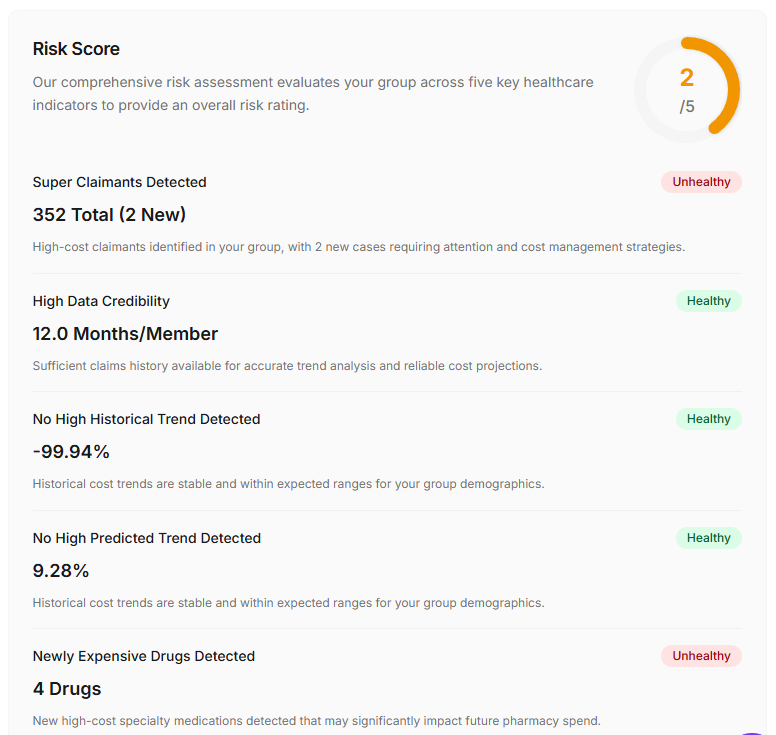
High-Cost Claimants
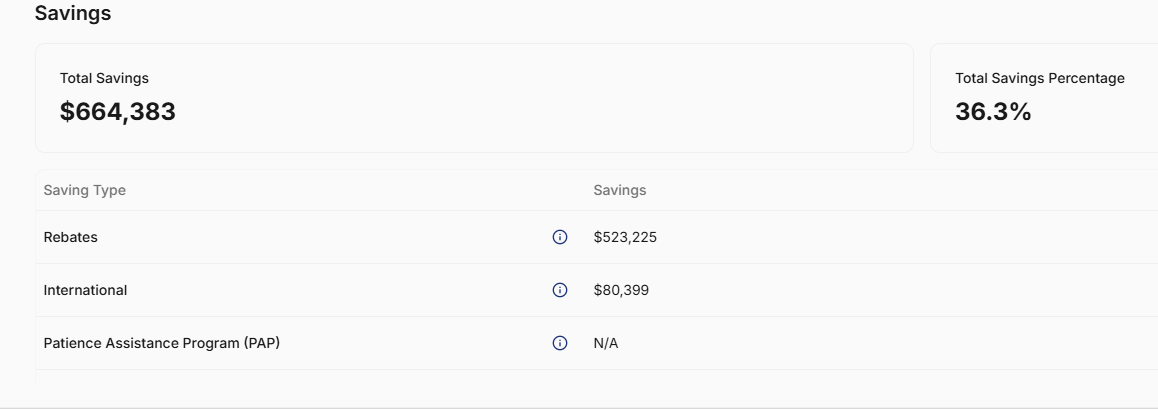
Minimum 20% Savings
with our Audit Tool
Before and After Drug Spend after Appro-Rx Audit and Consulting
Benefit Plan Assessment ✶
Benefit Plan Assessment ✶
Take control
of your pharmacy benefit spend with a
Appro-Intel Audit
-
Current PBM contract
Twelve-month file of claims and rebate activity.
Note: Plan sponsors are entitled by law to receive their claims data in a timely manner, even if a vendor suggests otherwise.
-
Independent review in minutes using real claim data, contract terms measured against industry standards, and factual financial outcomes.
Understand your true bottom line without assumptions, personal bias, or vendor influence.
Map contract language to real claim and rebate data
Show how definitions, pricing structures, specialty terms, and rebate mechanics translate into actual plan cost with supporting evidence
Clarify whether the plan is performing as intended
-
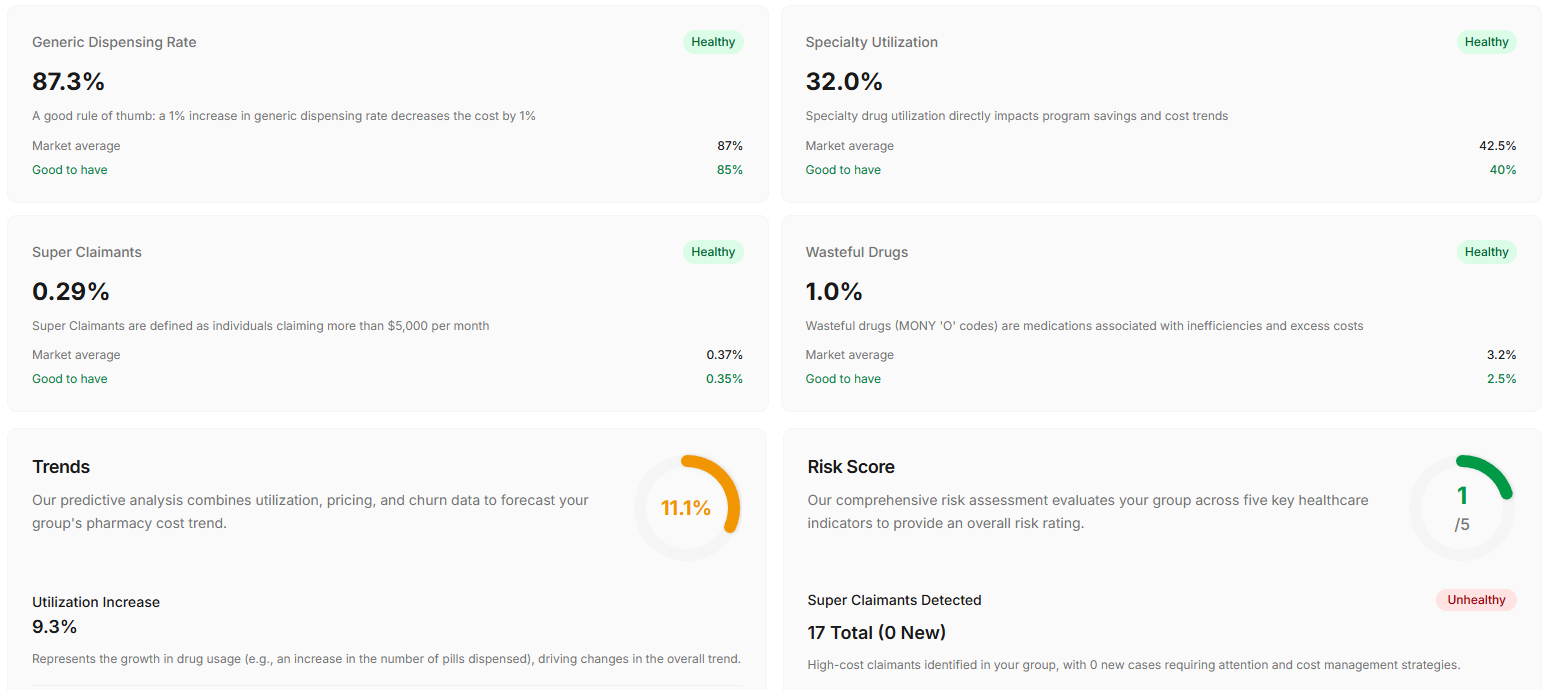
Net cost clarity
Trend analysis
Specialty impact
Hidden exposure areas
Biosimilar opportunities
Pricing inconsistencies
Where value is gained or lost
-
Renegotiate terms and correct weaknesses
Validate vendor performance
Capture savings while maintaining member access
Turn complex pharmacy economics into simple next steps
-
We walk you through the results and answer any questions.
You can use the findings to improve performance with your current PBM or explore Appro-Rx or trusted partners as an aligned alternative.
There is no risk and the potential for significant reward.
Plan Design Review ✶
Plan Design Review ✶
Take control
with our Pharmacist Designed, Guideline-Driven
Plan Design and Claim Review
-
Current PBM Formulary
Twelve-month file of claims and rebate activity
Note: Plan sponsors are entitled by law to receive their claims data in a timely manner, even if a vendor suggests otherwise.
-
Evaluates the pharmacy benefit through a clinical and economic lens
Applies pharmacist-led judgment to formulary and claims behavior
Surfaces how market dynamics influence cost and access
Frames opportunities around patient outcomes and benefit integrity
-
Net cost optimization opportunities
Specialty and generic utilization trends
Specialty impact on total spend and interchange opportunities
Lowest-net-cost formulary options
Biosimilar savings opportunities
Pricing inconsistencies across channels
Where value is gained or lost in the benefit structure
Prior authorization, quantity limit, and day supply optimization
-
Optimize existing plan design without disrupting member access
Use the plan’s own data to capture savings already within reach
Implement changes often avoided under traditional PBM models
Align decisions to true net cost rather than vendor incentives
-
Analyze how claims are adjudicated and how formulary rules are applied
Review drug selection logic, pricing methodology, and channel routing
Compare covered therapies to clinically equivalent alternatives
Evaluate the role of spread, rebates, and contractual incentives
Document divergence from lowest-net-cost execution
Walk through findings with a clear path to implementation
Connect With
A Sales Rep.
Andy.Suittor@ApproRx.com
Jordan.Mullins@ApproRx.com